Snake In Scratch
Here you have a scratch tutorial for a very fun game
This is a classic game it was actually one of the first pc games in the world, and it is the forefather of many popular games like slither.io and supersnake.io.
Her you can try snake on scratch
Instruction
CoderDojo Milltown – Scratch Exercise 2 – Snake – v1.0 Step 5 The final bits of code for the snake are on the right This tells the new cloned version of the sprite thats left behind to become a body costume (a cloned element is always a body) It then simply says to just wait (no movement) for the delay value by the length of the snake. Snake in the Eagle's Shadow (Chinese: 蛇形刁手) is a 1978 Hong Kong martial arts action-comedy film directed by Yuen Woo-ping in his directorial debut. It stars Jackie Chan, Hwang Jang Lee, and Yuen Woo-ping's real life father, Yuen Siu Tien. Right after this film, Yuen Woo-ping directed Drunken Master, released in the same year, which also starred Jackie Chan, Hwang Jang Lee and Yuen Siu. Typically, snakes need a lot of heat and some may also require humidity. You can heat your snake’s enclosure using lamps, heaters, mats or even rocks. These items may cost anywhere from $20 to $50 at the pet store. Don’t forget to budget for the monthly electricity expense that these items represent. Snake Bedding Costs. How to Create a Timer in Scratch Create a Timer Variable. Open the saved game project in Scratch. Select the sprite that you will use to track the time (it might be the player). From the Variables palette, click Make a Variable. Type timer as the variable name.
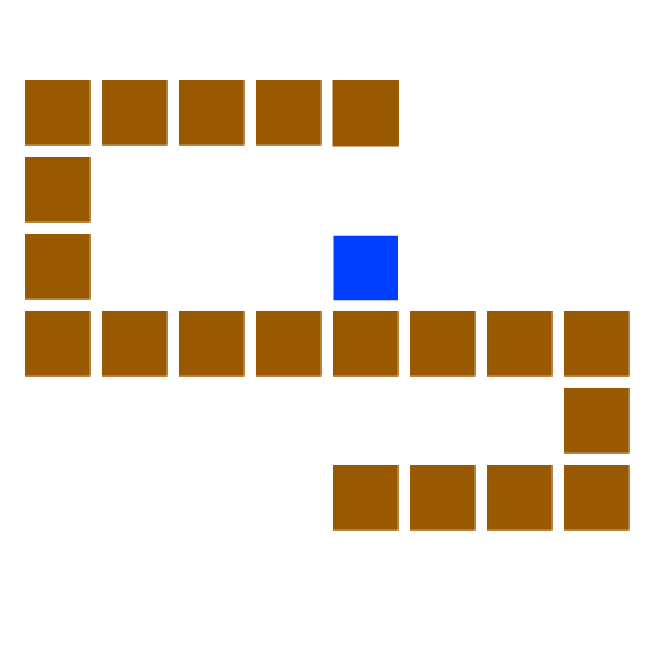
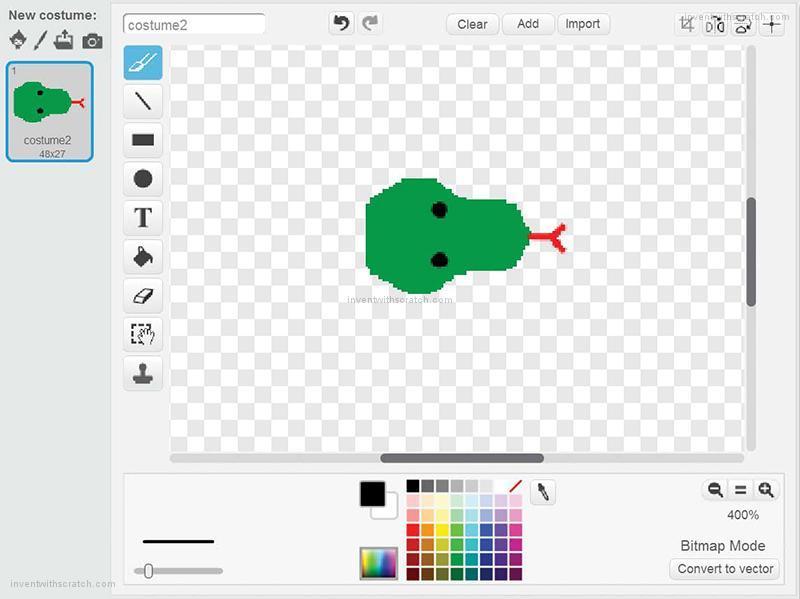
- Make 3 figures
Figure 1
- Make a button that is visible when the program start
- Add some code:
- When the button is clicked, hide it and broadcast “new game”
Figure 2
- Add first code:
- When I receive “New game”
- Hide
- Broadcast “Make New”
- Second code:
- When I receive “Make New”
- go to x “”14″*” pick random “-15” to “15”” y “”14″*” pick random “-10” to “10””
- create clone of “myself”
- clone code:
- When I start as a clone
- Show
- Wait until “touching “Figure 3”
- Change “Length” by “2”
- Brodcast “Make New”
- Delete this clone
Figure 3
- Add the first code:
- When start clicked go to x “-20” y “0” point in direction “-90”
- The second code you need to make is a test “if key (…) pressed point in direction (…)”
- Make one test for all the arrow keys and put it in an endless loop under “When I receive “new game””
- Third code is:
- Make 3 variables
- Time
- My time
- Length
- Start when I receive “new game”
- Sett “Time” to “0”, and “Length” to “5”
- Make a loop:
- Repeat until “touching “edge” or touching color “the color on your snake””
- Inside the loop
- Set “My time” to “Time”
- Change “Time” by “1”
- wait “0,1”secunds
- Create clone of “myself”
- move “14” steps
- Make a code for the clone:
- when I start as a clone
- Wait until “Time” – “Length” = “My time”
- Delete this clone

Abstract
Snake bites are one among the under reported clinical emergencies from tropical countries. There are variations in clinical presentation of snake bites and its toxic features differ with the species and type of bite. There are lots of controversies in the treatment guidelines which often makes it difficult to manage. We report the case of a severe hemotoxic snake bite who presented to the outpatient service of our hospital with a trivial foot injury. Even though snakebites are familiar clinical situations for an emergency physician from tropics, we report this case as most are under reported. We also intend to emphasize the excellent outcome of appropriately diagnosed and treated cases of snake bite.
1. Introduction
Snakebite is a major public health issue in the tropical and subtropical nations of South Asia, Southeast Asia, and sub-Saharan Africa–. Snake bites are among the common emergency room cases in the tropical countries. In developed nations, most of the snake bite occurs on recreational activities, whereas in developing countries it is more of an occupational disease. If the bites are identified early and managed appropriately, the morbidity and mortality from snake bites are negligible. We identified snake bite with severe coagulation failure in a patient, who came for tetanus toxoid injection for a trivial scratch on his left little toe. In 2010 World Health Organization has published the new guidelines on snake bite management for the South East Asian Countries[5].
2. Case report
A 40 year old truck driver visited the medical outpatient facility of our hospital for a tetanus toxoid injection. He had a scratch on his left little toe while getting down from the truck about an hour before. He had no significant illnesses in the past. On local examination (Figure 1) of the little toe the scratch appeared like fang marks, mild swelling was present and the area was warm to touch. There was no bleeding from the site. The general and systemic examination was unrevealing. There were no clinical features of haemo or neuro toxicity. The patient again was interviewed in detail on the mode of sustaining the scratch. He was unable to recollect or give a history suggestive of snake bite. He was re-examined and still had no features of haemotoxicity and neurotoxicity.
Blood samples were drawn immediately, and clotting time, whole blood clotting time and aPTT were found to be grossly prolonged. In view of the moist terrain from which he sustained the injury the possibility of snake bite was considered. After explaining on the possibility of a poisonous snake bite and obtaining high risk consent, he was started on polyvalent anti-snake venom (ASV) as per the WHO guidelines for severe coagulation failure. He was given supportive drugs and antibiotics.
After an hour of admission the patient complained of severe burning pain in the left leg. On examination, skin around the scratch had turned black and up to the knee the left leg was warm, tender and oedematous. He also had tender left sided inguinal lymphadenopathy. There were no active bleeding from any sites and neurological deficits. Over the next 24 hours the repeated clotting time, whole blood clotting time and APTT were normalized. The symptoms and signs pertaining to the left leg regressed over the next 96 hours and he was discharged from the hospital on day 7. Except for mild skin rashes on initiating the ASV, no other complications were noticed during the hospital stay.
3. Discussion
Snakebite is a common and potentially life-threatening condition in the tropical and subtropical nations of Asia and Africa. Among the 216 species of snakes seen in India, the commonly encountered venomous snakes are cobra, krait, Russell's viper and saw-scaled viper. Majority of these cases are seen in the monsoon months and in the age group 21–50 years (71%) as observed by Brunda et al. India is amongst the countries with high mortality due to snakebite, in spite of being the largest producer of ASV,. Due to poor reporting and lack of national registry the impact of snake bite in India is underestimated. These cases are potentially life threatening due to the haemotoxic, neurotoxic and myotoxic effects of the venom depending on the biting species.
As hemotoxic features were predominant in our patient and viper bites were common in the geographic area he possibly had a viperid envenomation. Venom contains different proteins such as enzymes, non-enzymatic polypeptide toxins, and non-toxic proteins. Enzymes constitute 80%-90% of viperid venom, which includes digestive hydrolases, hyaluronidase, and kininogenase. Venoms of Viperidae and some Elapidae and Colubridae contain serine proteases and other procoagulant enzymes which are thrombin-like or activate factor X, prothrombin and other clotting factors, stimulating blood clotting with formation of fibrin. This may paradoxically result in “consumption coagulopathy”. Viperidae venom contains multiple anti-haemostatic toxins that activate factors V, X, IX and XIII, fibrinolysis, protein C, platelet aggregation, anticoagulation and haemorrhage. Also the zinc metalloproteinases present in viperid venoms cause direct vascular endothelial damage and bleeding. These multiple factors cascade and contribute to the hemotoxicity, resulting in coagulopathy and spontaneous bleeding associated with viperid envenomation,.
Most patients with snake bite present to hospital with an unknown bite or with a bite from an unidentified species. It is a daunting challenge for an emergency department medical officer to identify an unknown bite and to identify the species from the bite mark. The most common clinical scenario is a suspected snake-bite, and many patients do not receive treatment or develop complications, due to under diagnosis or over diagnosis of snakebite with or without envenomation. In India, most cases are from rural areas and they are referred to higher centres resulting in a delay in initiating appropriate treatment.
Isbister et al noted suspected snakebite to be common and severe envenoming seen in less than 5% of bites. Tibballs tried to identify reliable predictors of envenomation in suspected snake bite and examined the standard of treatment in envenomed subjets. The common symptoms of headache, abdominal pain, nausea or vomiting, or abnormal coagulation tests or presence of local reaction, swelling, necrosis could predict envenomation. Bawaskar et al from India observed that the snakes causing the bite were mostly identified by the signs and symptoms, and also from the dead snakes brought along.
A thorough history, circumstances of bite, followed by a local and systemic examination often make it easy to diagnose snakebite,[5]. Ariaratnam proposed a syndromic approach to snake bite envenomations and our patient falls to syndrome-2 as had features of coagulopathy. Suchitra et al from South India, studied the clinical characteristics, factors for complications and the outcomes of snake bite in relation to timing of polyvalent ASV administration in patients with snakebite envenomation. Among the 586 cases studied, 34% had sustained outdoor bites and snake species was identified in 34.5% of bites. 93.5% of patients had signs of local envenomation and 61% had regional lymphadenitis.
The 20-min whole blood clotting test is a simple, rapid and reliable test of coagulopathy and also in assessing the effectiveness of ASV. Simpson emphasizes the need in providing guidance for the primary healthcare doctor in identification of medically significant snakes, treatment, and referral criteria. Snakebites can manifest with regional and systemic features based on the amount and type of venom injected during the bite, and at times the systemic manifestations occur much latter. In the present case initially there were no features of systemic envenomation but later had coagulopathy. This makes it essential to observe these bite victims for at least 24 hours prior to discharge from hospital.
Management of snake bite, initiation of therapy, type of ASV, its dosage have all been surrounded by controversies for decades,–,. The WHO guidelines for snakebite management in Southeast Asia (2010) clearly mentions on the indications and dosage of ASV[5]. Punde analyzed 633 patients with snake-bites and its management over a 10-year period. Of the 427 envenomed by poisonous snakes, 64.2% were by saw-scaled viper, 16.6% by cobra, 9.8% by krait and 9.4% by Russell viper. The average requirement of ASV was 40–320 mL for treating neurotoxic envenomation and 20–250 mL for Echiscarinatus and Russell viper bites.
Complications vary from neuroparalysis, hemolysis, coagulopathy, hypotension, renal failure, cellulitis to rhabdomyolysis. Suchitra et al noted complications in 39.5% of patients and acute renal failure (25.5%) was the commonest complication. They observed a mortality of 3%. Capillary leak syndrome, respiratory paralysis and intra cerebral bleeding were the common risk factors for mortality in their study. Also, patients who received ASV after 6 hours of bite had higher rate of complications. They observed the presence of leucocytosis and severe coagulopathy, as factors to predict adverse outcomes.
Inamdar et al from Central India studied the outcome, seasonal variation, and death pattern of snakebite cases over 10 years. They concluded snake bite as a life-threatening emergency; early appropriate use of antivenom and close monitoring will reduce complications and mortality.
Clinical knowledge of the varied manifestations is essential for effective management and prevention of complications in cases of snake bite.


In the developing and under developed nations, the delay in administration of ASV, poor primary health care, and difficulties with transportation from rural areas to major centres contribute to the high case-fatality ratio of snakebite envenomation. The hospitals in tropics should develop an admission policy of suspected snakebites to manage envenomation. The policy should encompass appropriate treatment with no early discharges and no non-envenoming bites treated with ASV.
Footnotes
Conflict of interest statement: We declare that we have no conflict of interest.
References
Snake Game In Scratch 3.0
Snake Scratching Head
How To Make A Snake In Scratch
